In this blog, Gini Melesi, Head of Transformation, East of England Cancer Alliance, & Diane Whitney, Head of Brachytherapy Physics, Cambridge University Hospitals NHS Foundation Trust, explore the relationship between health literacy, shared decision making and patient outcomes in cancer.
For patients with cancer, being given access to personalised information resources can have a significant impact on their quality of life. This was recognised in the 2019 NHS Long Term Plan for Cancer, which stipulated that every person diagnosed with cancer should have access to personalised care – including needs assessment, a care plan and health and wellbeing information and support[1].
However, patients are too often expected to understand complicated information about their diagnosis and management in order to participate in their own treatment and care. This is a huge challenge for those without the personal characteristics and social resources to access, understand, and appraise the information they are provided with[2] (the WHO definition of health literacy). A systematic review of health literacy in cancer care concluded “Those with lower health literacy face greater difficulties processing information, report poorer psychological outcomes and experience a poorer quality of life”[3]
This article gives evidence for the importance of considering health literacy when designing patient education and shared decision making resources for patients with cancer. It looks specifically at how the management of prostate cancer is evolving and changing to improve patient options, and how the East of England Cancer Alliance has responded to adopt the recommendations and adapt to those changes for the benefit of all patients with a new prostate cancer diagnosis.

Information powering shared decision making
Good patient education and information improves health outcomes whilst reducing time and resource burdens on clinicians and care services[4]. Patients need to understand the options available and why a particular treatment plan is recommended to them. In the case of cancer care, it’s especially important that patients are given the opportunity to fully understand their diagnosis, how it will impact their lives, and their treatment options and journey[5]. This can help reduce anxiety and reassure family members at a highly stressful time. Providing bias-free, clear and factual information also enables shared decision making between patients and clinicians and the giving of informed consent[6].
Barriers to effective communication
There are a number of common roadblocks that reduce the impact of education initiatives. Foremost amongst these is accessibility. Not all patients have the technology or the digital literacy to navigate complex online resources, and few people can decipher the acronyms and technical terminology that can feature heavily in patient guides. According to census data, 1.5% of the population of the UK cannot speak English ‘well’, which means they rely on translations from friends or family members if they are only provided with English language resources. Due to the complex nature of health information, poor health literacy affects a large proportion of the population. 61% of England’s working-age population find health information difficult to understand, and studies have found that 40% to 80% of the information given during appointments is forgotten immediately. If ‘too much’ information is presented to patients at once, and a large amount of that information is not relevant to their unique circumstances, it becomes very difficult for the patient to isolate and digest the information they need.
The challenge for organisations such as the NHS Cancer Alliances, which strive to support information provision to cancer patients, is how to most effectively communicate relevant information without introducing bias or influencing decision making.
Unique amongst Cancers
Prostate cancer is unique in that it has more than one common treatment pathway available to the patient, including active surveillance, surgery, radiotherapy, brachytherapy and hormone therapy. Treatments have different risks and side effects and sometimes there is no compelling evidence that one option is superior to another with regards to success and outcomes, but they do have very different impacts on the patient’s quality of life[10].

Options are available to all patients but there are factors that influence their choice of treatment option – such as geography – i.e. the distance they may need to travel to access some options, their age, lifestyle and BMI, and the details of their diagnosis. Usually patients themselves still make the ultimate decision on which treatment to proceed with. This can be daunting and access to unbiased information and recommendations is vital.
For example, for very low stage prostate cancer, the recommended option is Active Surveillance i.e. no active treatment at all. This can be a difficult concept for someone being told they have cancer – that the best option for them might NOT be to remove it. It is important to educate a patient that their risks are low, they will be well monitored and that living without the side effects of treatment might be their best option. Balancing this with the importance of close monitoring until treatment is clinically indicated or requested and accepting that the potential physiological challenges of living with cancer may be prohibitively difficult for some patients.
New NICE Guidelines for the Diagnosis and Management of Prostate Cancer
In 2021, the National Institute of Health and Care Excellence, NICE implemented new risk stratification definitions for prostate cancer[11].
Linked to this publication were NICE shared decision making guidelines recommending Health Professionals to use patient decision aids as one part of an overall ‘toolkit’ to support shared decision making[12], defined as “a collaborative process that involves a person and their healthcare professional working together to reach a joint decision about care”.
In response, the East of England Cancer Alliance identified issues with patient information and informed consent and agreed to fund a decision tool to translate the updated NICE guidelines into a patient accessible website. The aim was to build a tool that would support patients diagnosed with prostate cancer who are faced with multiple choices and sources of information.
The result was the Prostate cancer: knowing your options website. This is the first tool that provides men with “direct to patient” NICE guideline recommendations, in an easy to understand and independently accessible format. It is now also endorsed by PCUK Resources for your patients | Prostate Cancer UK.
Building for accessibility: putting patients in the driving seat
We were mindful of the importance of creating resources accessible by patients with varying levels of health literacy. Because of this, patient involvement was an important consideration in the development of the tool. From the outset of development, the East of England Cancer Alliance consulted with the “Together Against Cancer” Norfolk and Norwich University Hospital prostate cancer focus group, who gave invaluable feedback on accessibility and language for the website prototypes.
Ideally, patients should be brought in as early as possible in the design and planning process, so that the right direction is taken in terms of content structure and the medium of delivery. Waiting to secure the patient perspective on a nearly finished product means that any suggested amends will be costly and more complicated to deliver.
The East of England Cancer Alliance listened carefully to the group’s feedback that the unbiased NICE guideline data was informative, but that visual and video aids would be a useful addition.
For the video learning content on the site, Cognitant Group was brought in as specialists in patient engagement. Drawing on their experience designing patient-centric learning programmes, they ran workshops with patient stakeholders from the Norwich prostate patient group, as well as healthcare professionals from the region, to ensure that the tool provided answers to the most pressing and commonly-asked patient questions. Patient input was sought to inform the content design and build to ensure that the programme was accessible and valuable to its target audience, and to ensure that the most salient points were communicated with impact without risking information overwhelm.
Once launched, patient feedback was also sought, with audit returning positive results:
- 88% respondents found website useful
- 84% used independently at home
- 84% said it helped them understand diagnosis better
- 84% would recommend to other patients in their position
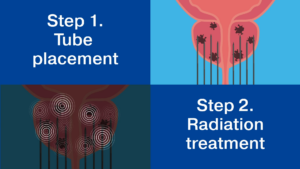


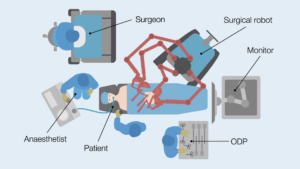
Images from patient-centric learning programmes designed by Cognitant
Individual responses were positive, with a number specifically backing up the drive for standardised patient information for all patients with a new prostate cancer diagnosis.
By continually seeking and integrating patient feedback, we can ensure that our patient information resources meet Health Literacy standards and remain relevant and effective.
Improving prostate cancer outcomes
As we have explored, the complexity of cancer care information poses significant challenges for patients, particularly those with limited health literacy. This is why, in order to improve outcomes for patients, shared decision aids must be tailored to the health literacy and accessibility needs of the intended audience. By prioritising co-creation with patients and experts, such initiatives drive better health outcomes by empowering patients with cancer to be well-informed and active participants in their care journey.
References
[1] “NHS Long Term Plan » Cancer.” NHS Long Term Plan, https://www.longtermplan.nhs.uk/online-version/chapter-3-further-progress-on-care-quality-and-outcomes/better-care-for-major-health-conditions/cancer/. Accessed 2 January 2024.
[2] “Health literacy toolkit for low- and middle-income countries.” World Health Organization (WHO), https://www.who.int/publications/i/item/9789290224754. Accessed 2 January 2024.
[3] Holden CE, Wheelwright S, Harle A, Wagland R (2021) The role of health literacy in cancer care: A mixed studies systematic review. PLoS ONE 16(11): e0259815. https://doi.org/10.1371/journal.pone.0259815
[4] Paterick TE, Patel N, Tajik AJ, Chandrasekaran K. Improving health outcomes through patient education and partnerships with patients. Proc (Bayl Univ Med Cent). 2017 Jan;30(1):112-113. doi: 10.1080/08998280.2017.11929552. PMID: 28152110; PMCID: PMC5242136.
[5] McPherson, Christine & Higginson, Irene & Hearn, Julie. (2001). Effective methods of giving information in cancer: a systematic literature review of randomized controlled trials. Journal of public health medicine. 23. 227-34. 10.1093/pubmed/23.3.227.
[6] Paterick TE, Patel N, Tajik AJ, Chandrasekaran K. Improving health outcomes through patient education and partnerships with patients. Proc (Bayl Univ Med Cent). 2017 Jan;30(1):112-113. doi: 10.1080/08998280.2017.11929552. PMID: 28152110; PMCID: PMC5242136.
[7] “Language, England and Wales: Census 2021.” Office for National Statistics, 29 November 2022, https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/language/bulletins/languageenglandandwales/census2021. Accessed 20 October 2023.
[8] Local action on health inequalities: improving health literacy.” GOV.UK, 15 September 2015, https://www.gov.uk/government/publications/local-action-on-health-inequalities-improving-health-literacy. Accessed 20 October 2023.
[9] Kessels, Roy PC. “Patients’ memory for medical information – PMC.” NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC539473/. Accessed 20 October 2023.
[10] https://www.nice.org.uk/guidance/ng131/chapter/Recommendations
[11] Recommendations | Prostate cancer: diagnosis and management | Guidance.” NICE, 9 May 2019, https://www.nice.org.uk/guidance/ng131/chapter/Recommendations#staging. Accessed 2 January 2024.
[12] “Overview | Shared decision making | Guidance.” NICE, 17 June 2021, https://www.nice.org.uk/guidance/ng197. Accessed 2 January 2024.
[13]https://www.macmillan.org.uk/_images/lets-talk-about-it-improving-information-and-support_tcm9-300548.pdf
Cognitant
Looking to empower people with health information for better patient outcomes?
Related News
Kidney Research UK invests in Healthinote patient education platform which could support >15m people with long term health conditions
April, 2025
Oxford, January 2025 – Kidney Research UK, the leading charity dedicated to kidney health, has made a significant investment in Cognitant Group Ltd, a leading...
Webinar Insights – Compliance vs Patient Engagement: Can They Co-Exist?
April, 2025
Is compliance really a barrier to meaningful patient engagement in pharma, or are outdated myths holding us back? In this recent webinar, Dr Tim Ringrose,...
Funding awarded to innovations that support early diagnosis and rehabilitation of Stroke patients
March, 2025
SBRI Healthcare, an Accelerated Access Collaborative (AAC) initiative, in partnership with the Health Innovation Network, has awarded £2.5 million for the development of five innovations...